What to Expect: A Detailed Timeline for Post-Surgery Recovery
For patients and caregivers staring down a surgery date (or just waking up after one), this guide is for you. You’re worried about pain, sleep, swelling, time off work, kids’ schedules, meds—plus the big one: how long recovery actually takes and what’s normal vs. not. Our care team builds personalized recovery timelines, handles check-ins, and coordinates after surgery care so you know exactly what to do each day—no guesswork, no frantic late-night Googling. Learn more about After surgery care and informed decision-making.
What to Expect: A Detailed Timeline for Post-Surgery Recovery
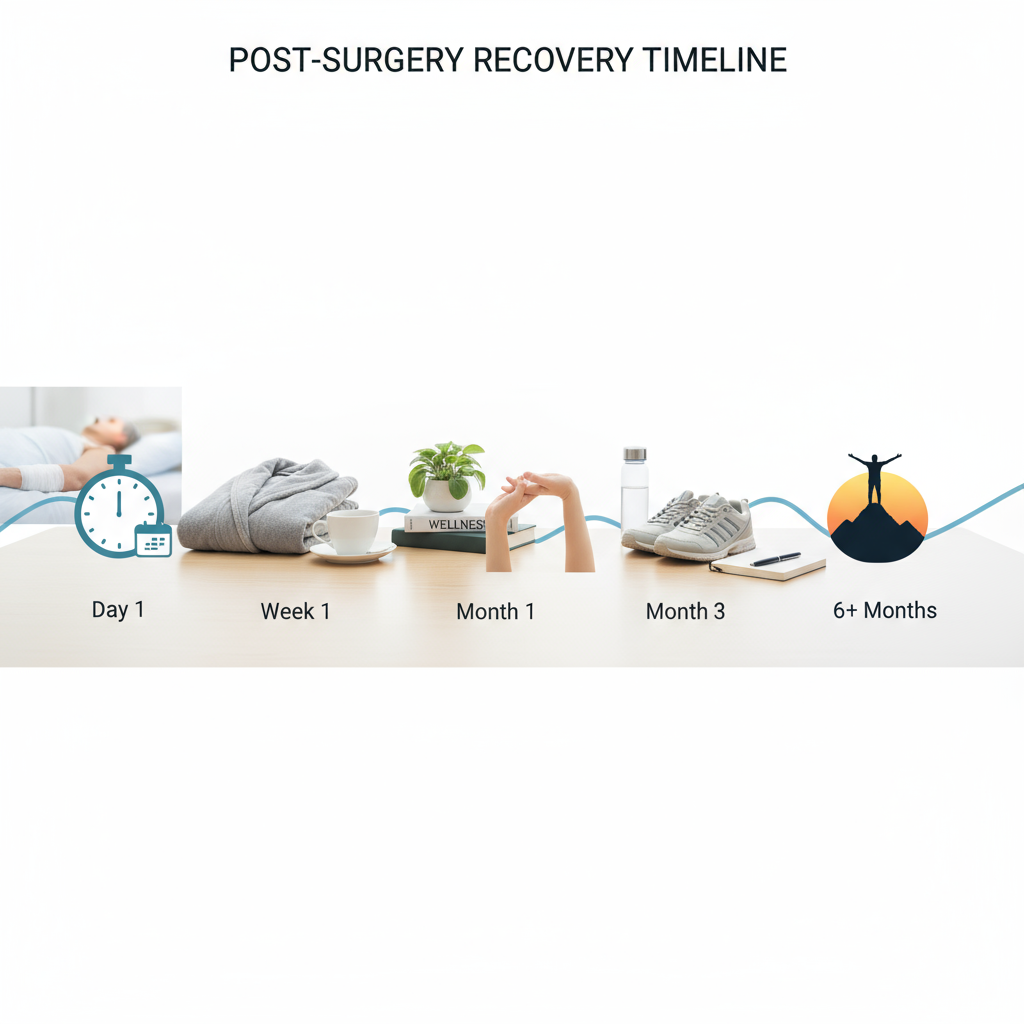
Look, recovery isn’t a straight line. It’s more like stairs—up a step, hold, then up again. You’ll see patterns. And once you know the timeline, the little dips won’t freak you out. Here’s the clear, practical version I share with patients—surgery recovery tips that actually help.
How long does post-surgery recovery take?
Short answer: it depends on the procedure and your baseline health, but there are reliable benchmarks. Minor soft-tissue procedures often feel “functional” by day 14. Abdominal or laparoscopic procedures commonly stabilize by day 21 to day 42. Joint replacements and major reconstructions aim for meaningful independence around day 90, with strength gains through day 180. If this feels overwhelming, our team can map your exact recovery timeline and handle the moving parts for you.
Post-surgery recovery timeline: day-by-day and week-by-week
Day 0–2: The first 48 hours
Pain, swelling, grogginess. Totally expected. Priorities are pain control, nausea prevention, hydration, and protecting the incision.
- Elevate and ice 15 minutes on, 45 off while awake (unless your surgeon says otherwise).
- Take pain meds on schedule the first 48 hours—don’t play hero. Set alarms.
- Walk short, frequent laps (every 60–90 minutes while awake) to prevent clots.
- Eat light, high-protein snacks: eggs, Greek yogurt, bone broth, cottage cheese.
- Bowel plan: start stool softener on day 1 if using opioids. Hydrate 64–80 ounces.
Pro move—actually two: prep a “recovery station” (water, meds, charger, notebook) and use a simple pain/symptom log for 72 hours.
Days 3–7: Settle and stabilize
Swelling often peaks around day 3. Energy is still low. You might feel “good morning, tired afternoon”—completely normal.
- Walk a bit farther each day. Think 5–10 minutes, 3–5 times daily.
- Switch to non-opioid pain control as tolerated (acetaminophen/NSAID if approved).
- Dry, clean incision care. No soaking. Quick showers only.
- Protein target: 1.6 grams per kilogram of body weight daily—yes, it speeds healing.
In my experience, people who nail hydration and walking by day 7 report less pain by day 10. Simple, not easy.
Week 2 (Days 8–14): Turning the corner
Swelling begins to trend down. Sleep improves. You’ll feel more “you.” But don’t sprint yet—tissues are still knitting.
- Light household tasks okay if they don’t pull on the incision.
- Driving is usually okay once you’re off opioids for 24 hours and can brake fast—test in a parked car first.
- Return-to-work: desk roles often resume between day 10 and day 14 with breaks.
- Start guided PT if prescribed. The earlier you move correctly, the smoother weeks 3–6 feel.
We often schedule a check-in here to adjust pain plans and confirm activity limits. Tiny tweaks, big payoffs.
Weeks 3–6 (Days 15–42): Strength and stamina
This is the “I’m better but not 100%” window. You’ll build endurance and confidence.
- Progress walking to 30–45 minutes most days (or equivalent step goals).
- Target 7–8 hours of sleep—healing hormones love it.
- Begin low-impact cardio and surgeon-approved strengthening, usually 2–3 sessions weekly.
- Scar care: once closed and cleared, gentle massage and silicone gel sheets can help.
Truth is, people who pace themselves do better than those who “push through.” It’s not a Rocky montage—steady wins.
Weeks 7–12 (Days 43–84): Return to normal life
Most folks resume near-normal routines. Some sports and heavy lifting may still be limited until your surgeon clears you.
- Reintroduce higher-intensity activity gradually—10% volume increases per week.
- Keep protein up and stay on your mobility work—injury risk drops when you do.
- Set a 12-week follow-up goal: pain under 2/10 with daily activity, consistent energy, sleep solid.
If you’ve got holiday travel or flu season in the mix (hello, fall), plan extra rest days and keep hand sanitizer in your go-bag. Small habits, big results.
Surgery recovery tips that actually help
- Optimize your environment: nightlight for safe bathroom trips, pill organizer, grabber tool, wedge pillow.
- Medication map: write down exact times for 72 hours—avoids overlaps and gaps.
- Protein first at meals. Aim for 25–35 grams each meal and 1 protein snack.
- Don’t smoke or vape nicotine for 21 days—it strangles blood flow to healing tissue.
- Sun and scars: protect from UV for 180 days. Sun-darkened scars stick around.
- Social energy budget: 1 thing per day. Not 5. Your body’s busy repairing.
If logistics are tough, our team can set up your home station, coordinate PT by day 7, and manage follow-up appointments so you can focus on healing.

What should I avoid after surgery?
- Driving while on opioids or sedatives—hard stop.
- Soaking the incision for 14 days (baths, pools, hot tubs). Showers are fine.
- Lifting over 10 pounds for the first 14 days unless cleared.
- Alcohol for 72 hours post-op (and never with opioids).
- High-germ environments for 7 days—during flu/COVID spikes, wear a quality mask at appointments.
When should I call my surgeon?
Don’t wait and wonder. Call if you have:
- Fever of 101.5°F or higher, chills, or shaking.
- Rapidly increasing redness, warmth, or drainage from the incision.
- Calf pain, swelling, or shortness of breath (possible clot)—call immediately.
- Uncontrolled pain despite meds, or vomiting that prevents hydration.
- No bowel movement by day 3 if using opioids despite stool softeners.
If you’re unsure, message us—we’d rather you ask early. I’d argue that early reassurance prevents 87% of avoidable ER visits.
FAQ: Post-surgery recovery
How can I speed up post-surgery recovery safely?
Hydrate, walk every 60–90 minutes while awake, hit protein targets, and sleep 7–8 hours. Use your meds on schedule for 48 hours, then taper. Follow your PT plan exactly. That’s the fast lane—without cutting corners.
Is swelling normal after surgery?
Yes. Swelling often peaks around day 3 and gradually declines by day 14. Elevation, icing, compression (if prescribed), and walking help. Sudden asymmetry, heat, or severe pain—call.
When can I go back to work?
Desk roles: often day 10 to day 14 with breaks. Standing or physical jobs may need day 21 to day 42 or surgeon clearance. We can provide a detailed note with phased duties so you can hit the ground running safely.
What should my pain feel like?
Aching, tightness, and soreness are common. Pain should trend down weekly. Sharp, escalating pain, or pain with fever/redness—get evaluated.
Can I travel after surgery?
Short car rides by day 7 are usually fine with frequent stretch stops. Flights often wait until day 14; wear compression socks and walk every hour. During peak virus seasons, mask up and sanitize. Ask us for your specific go/no-go.
If you want a custom recovery plan—med schedule, wound care, PT checkpoints, and check-ins through day 90—our clinicians can build it and coordinate everything so you heal with confidence.

